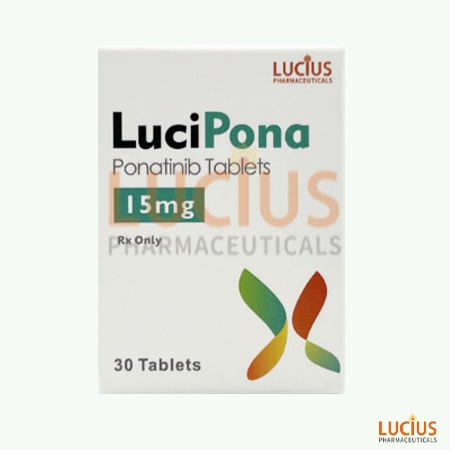
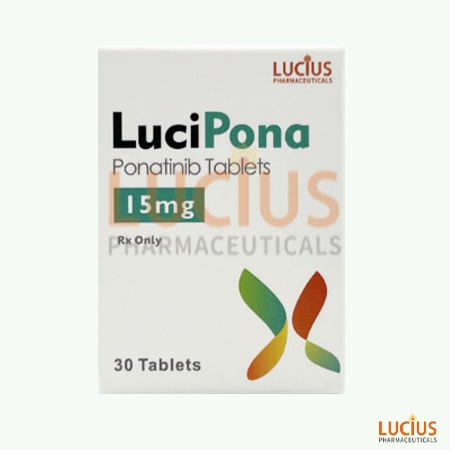
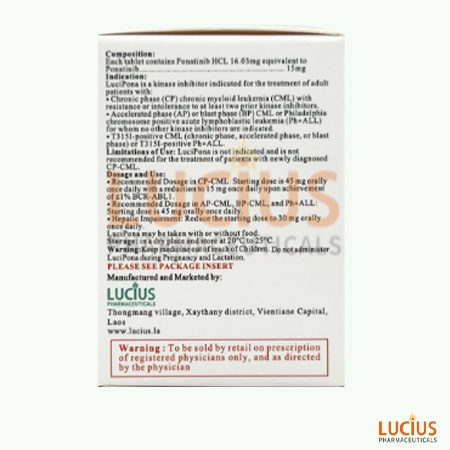
Another NamePonaxen、普纳替尼、Iclusig
IndicationsLeukemia
Reg No.04 L 1090/24
Inspection NO.0671-24
Ponatinib is a kinase inhibitor indicated for the treatment of chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) and chronic myeloid leukemia (CML) in Philadelphia.
It is also necessary to pay attention to the possible adverse reactions and precautions during use. When purchasing, be sure to choose a formal channel to ensure the quality and safety of the drug.
Ponatinib is a drug used to treat leukemia. It belongs to tyrosine kinase inhibitors that block the proliferation and survival of leukemia cells by inhibiting abnormal tyrosine kinase activity in leukemia cells. Ponatinib is indicated for the treatment of chronic myeloid leukemia and Ph+ acute lymphoblastic leukemia, especially in patients who tolerate or cannot tolerate other therapeutic agents.
ponatinib
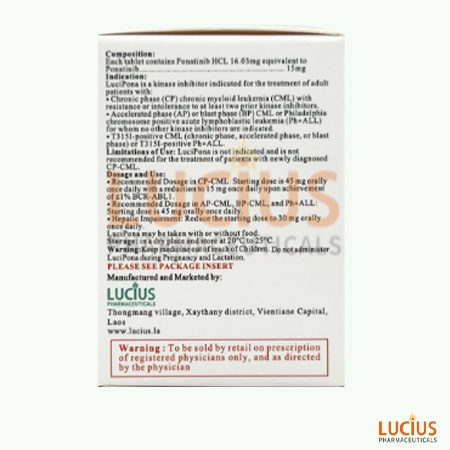
Ponatinib is indicated for the treatment of adult patients with:
2.1 Chronic phase (CP) chronic myeloid leukemia (CML) with resistance or intolerance to at least two prior kinase inhibitors.
2.2 Accelerated phase (AP) or blast phase (BP) CML or Philadelphia chromosome positive acute lymphoblastic leukemia (Ph+ ALL) for whom no other kinase inhibitors are indicated.
2.3 T315I-positive CML (chronic phase, accelerated phase, or blast phase) or T315I-positive Ph+ ALL.
Based on findings in animals and its mechanism of action, Ponatinib can cause fetal harm when administered to a pregnant woman. There are no available data on Ponatinib use in pregnant women. In animal reproduction studies, oral administration of ponatinib to pregnant rats during organogenesis caused adverse developmental effects at doses lower than human exposures at the recommended human dose. Advise pregnant women of the potential risk to a fetus. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. The background risk in the U.S. general population of major birth defects is 2 to 4% and of miscarriage is 15 to 20% of clinically recognized pregnancies.
There is no data on the presence of ponatinib in human milk or the effects on the breastfed child or on milk production. Because of the potential for serious adverse reactions in the breastfed child from ponatinib, advise women not to breastfeed during treatment with Ponatinib and for 6 days following the last dose.
Ponatinib can cause fetal harm when administered to pregnant women.
Verify the pregnancy status of females of reproductive potential prior to initiating Ponatinib.
Advise females of reproductive potential to use effective contraception during treatment with Ponatinib and for 3 weeks after the last dose.
Based on animal data, ponatinib may impair fertility in females of reproductive potential. It is not known whether these effects on fertility are reversible.
Safety and effectiveness have not been established in pediatric patients.
Of the 94 patients with CP-CML who received Ponatinib at a starting dose of 45 mg in OPTIC, 17% were 65 years and older and 2.1% were 75 years and older. Patients aged 65 years and older had a lower ≤1% BCR-ABL1IS rate at 12 months (27%) as compared with patients less than 65 years of age (47%). AOEs occurred in 38% (6/16) of patients 65 years and older and 9% (7/78) of patients less than 65 years of age.
Of the 449 patients who received Ponatinib in PACE, 35% were 65 years and older and 8% were 75 years and older. In patients with CP-CML, patients aged 65 years and older had a lower major cytogenetic response rate (40%) as compared with patients less than 65 years of age (65%). In patients with AP-CML, BP-CML, and Ph+ ALL, patients aged 65 years and older had a similar hematologic response rate (45%) as compared with patients less than 65 years of age (44%). AOEs occurred in 35% (54/155) of patients 65 years and older and in 21% (61/294) of patients less than 65 years of age.
Patients aged 65 years or older are more likely to experience adverse reactions including vascular occlusion, decreased platelet count, peripheral edema, increased lipase, dyspnea, asthenia, muscle spasms, and decreased appetite. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Patients with hepatic impairment are more likely to experience adverse reactions compared to patients with normal hepatic function. Reduce the starting dose of Ponatinib for patients with pre existing hepatic impairment (Child-Pugh A, B, or C). The safety of multiple doses, or doses higher than 30 mg, has not been studied in patients with hepatic impairment.
Overdoses with Ponatinib were reported in clinical trials. One patient was estimated to have been administered 540 mg via nasogastric tube. Two hours after the overdosage, the patient had an uncorrected QT interval of 520 ms. Subsequent ECGs showed normal sinus rhythm with uncorrected QT intervals of 480 ms and 400 ms. The patient died 9 days after the overdosage from pneumonia and sepsis. Another patient self-administered 165 mg on Cycle 1 Day 2. The patient experienced fatigue and non-cardiac chest pain on Day 3. Multiple doses of 90 mg per day for 12 days in a patient resulted in pneumonia, systemic inflammatory response, atrial fibrillation, and a moderate pericardial effusion.
In the event of an overdosage, stop Ponatinib, observe the patient and provide supportive treatment as appropriate.
Store Ponatinib tablets at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F)
Ponatinib administered to patients with cancer exhibited approximately dose proportional increases in both steady-state Cmax and AUC over the dose range of 2 mg to 60 mg (0.04 to 1.33 times the approved recommended starting dose). The mean (CV%) Cmax and AUC(0-24) of Ponatinib 45 mg orally once daily at presumed steady-state in patients with advanced hematologic malignancies were 73 ng/mL (74%) and 1253 ng•hr/mL (73%), respectively. Exposure increased by approximately 90% (median) [range: 20% to 440%] between the first dose and presumed steady-state.
The absolute bioavailability of ponatinib is unknown. Peak concentrations of ponatinib are observed within 6 hours after Ponatinib oral administration.
Effect of Food: Following ingestion of either a high-fat (approximately 900 to 1000 calories with approximately 150, 250, and 500 to 600 calories derived from protein, carbohydrate, and fat, respectively) or low-fat meal (approximately 547 calories with approximately 56, 428 and 63 calories derived from protein, carbohydrate, and fat, respectively) by 22 healthy volunteers, plasma ponatinib exposures (AUC and Cmax) were not different when compared to fasting conditions.
Ponatinib is greater than 99% bound to plasma proteins in vitro. There was no plasma protein binding displacement of ponatinib (145 nM) in vitro by other highly protein bound medications (ibuprofen, nifedipine, propranolol, salicylic acid, and warfarin).
The mean (CV%) apparent steady-state volume of distribution is 1,223 liters (102%) following oral administration of Ponatinib 45 mg orally once daily for 28 days in patients with cancer.
The mean (range) terminal elimination half-life of ponatinib was approximately 24 (12 to 66) hours following Ponatinib 45 mg orally once daily for 28 days in patients with cancer.
At least 64% of a dose undergoes Phase I and Phase II metabolism. CYP3A4 and to a lesser extent CYP2C8, CYP2D6 and CYP3A5 are involved in the Phase I metabolism of ponatinib in vitro. Ponatinib is also metabolized by esterases and/or amidases.
Following a single oral dose of radiolabeled ponatinib, approximately 87% of the radioactive dose was recovered in the feces and approximately 5% in the urine.
FDA,2022.02